Abstract

Sickle cell disease (SCD) is one of the most common inherited disorders in Saudi Arabia with nearly 60,000 affected individuals (Alsultan et al. Ped. Transplant. 2016). Allogeneic hematopoietic stem cell transplantation (HSCT) is a curative treatment in SCD. A recent international survey showed excellent long-term survival of SCD patients after HLA-identical sibling HSCT; however, patients aged 16 years or older had higher risk of GVHD and mortality (Gluckman et al. Blood 2017). HLA-identical related HSCT in adult SCD patients using non-myeloablative (NMA) conditioning consisting of alemtuzumab, 300 cGy total body irradiation (TBI), and sirolimus was successful in establishing long term stable donor chimerism with minimal toxicity and GVHD (Hsieh et. al. JAMA 2014). In this study, we reviewed the outcome of SCD patients who underwent transplant at our institution using standard protocols (NMA regimen in patients ≥14 years and myeloablative regimen in < 14 years) to address whether age remains a risk factor that influences HSCT outcome in SCD.
Children (<14 years) with severe SCD received myeloablative conditioning using one of two regimens: first regimen was cyclophosphamide (Cy) 200mg/kg, busulfan (Bu) 16mg/kg, and thymoglobulin (ATG) 10mg/kg and recently we use thiotepa 8mg/kg, Bu 16mg/kg, and fludarabine (Flu) 160mg/m2. Bu pharmacokinetics was performed to target AUC of 900-1350 µmol/L.min. GVHD prophylaxis included cyclosporine and methotrexate 10mg/m2 on day +1, +3, and +6. Bone marrow was the source of stem cells in all pediatric patients. Cyclosporine was continued during the first-year post HSCT and tapered slowly afterward based on donor chimerism. Adult patients (≥14 years) received hydroxyurea at maximum tolerated dose and hypertransfusion for 2-3 months with iron chelation if indicated prior to HSCT followed by NMA conditioning consisting of alemtuzumab (1mg/kg divided over 5 days on day -7 to -3) and TBI 300 cGy with testicular shielding in males on day -1. Sirolimus was used as GVHD prophylaxis starting day -2 and continued for at least one-year post HSCT with subsequent taper based on donor chimerism. Stem cells source was GCSF mobilized peripheral blood stem cells in all adult patients targeting cell dose of CD34 10X106/kg based on recipient weight. All SCD patients underwent exchange transfusion prior to HSCT to achieve HbS <30%. Hemoglobin was maintained between 9-11 g/dL and platelet count > 50,000/uL during HSCT. Supportive care included penicillin V, acyclovir, antifungal, and Pneumocystis jiroveci pneumonia prophylaxis. Levetiracetam was used as seizure prophylaxis. Strict monitoring of blood pressure and magnesium was performed. Graft failure and death from any cause were considered as events.
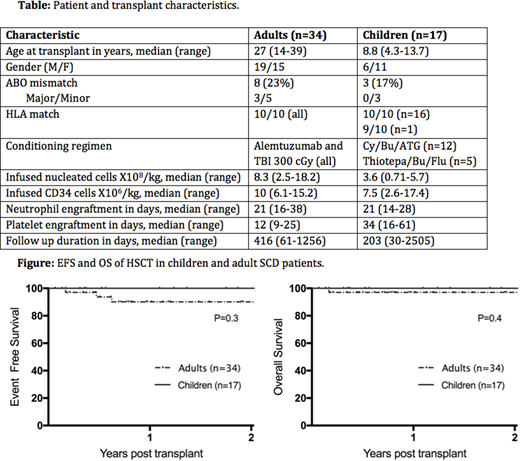
A total of 51 patients with severe SCD were transplanted at our center, 17 children and 34 adults. Patient and transplant characteristics are summarized in Table. Indications for HSCT included recurrent severe pain crisis (n=33), stroke (n=14), avascular necrosis (n=2), sickle cell hepatopathy (n=1), and priapism (n=1). All patients engrafted successfully for both neutrophil and platelets. There was no acute or chronic GVHD among adult patients. Two pediatric patient had mild grade I acute GVHD in the skin that was controlled with topical treatment and none of pediatric patients had chronic GVHD. Three adult patients developed secondary graft failure on day 61, 170, and 225 post transplant with aplastic marrow in two patients despite full donor chimerism and autologous recovery in the third patient. Among the two patients who had aplastic anemia, one died secondary to sepsis and one underwent successful second transplant using cyclophosphamide, Flu, and ATG. Thirty-one adults have stable donor chimerism. Event free survival (EFS) at 2 years was 90% in adult patients and 100% in children (P=0.3). Overall survival (OS) at 2 years was 97% in adults and 100% in children (P=0.4). Median follow up duration was 416 days (range, 61-1256) in adults and 203 (range, 30-2505) days in children.
We demonstrated that age-adapted approach in guiding the choice of conditioning regimen intensity in severe SCD is associated with excellent outcome and minimal risk of graft rejection, GVHD, and transplant-related mortality. This real world data is important to encourage patients and transplant physicians to consider this curative treatment. Longer follow up duration is needed to confirm our findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal